Our Process
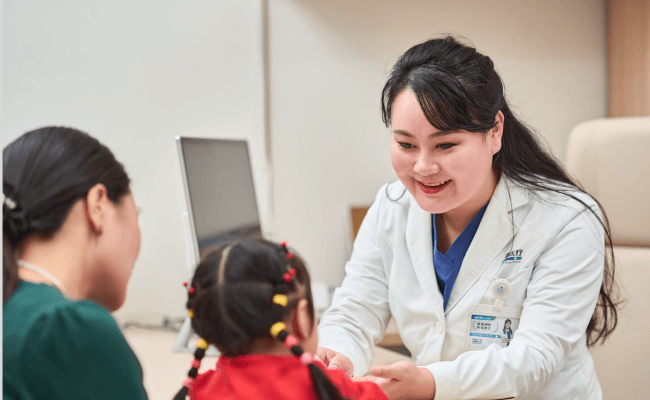
Initial Visit & File Creation
Scar Assessment
Personalized Treatment Plan
Treatment Tracking
Rehabilitation Guidance
Follow-up Tracking
Full-Cycle Health Follow-Up

Online Follow-up
System reminders and self-check guides via our app.
In-Person Follow-Up
We regularly assess your progress and adjust treatment plans as needed.

Home Rehab Guidance
Access to video courses, instruction manuals, and online Q&A.

Recurrence Management Promise
Should recurrence happen, continued treatment is provided at no extra charge.
Mental & Rehab Support
Psychological Counseling
We offer emotional assessments and professional counseling support (by appointment).
Peer Support Program
"Scar Friends Home" groups allow patients to share experiences and support one another.

Functional Training Guidance
Our professional physical therapy team provides guidance on functional rehabilitation exercises.
Patient Guide
Can keloid treatment be done during pregnancy?
No! It is recommended to undergo treatment after giving birth. Why is this so? In clinical practice, many of the keloid patients we see experience rapid growth of their keloids during pregnancy. Before pregnancy, the keloids are in a relatively stable phase and grow slowly. However, after pregnancy, once the hormone levels in the body change, the keloids can grow rapidly and become more severe. Therefore, we recommend that female patients who have keloids and are planning to get pregnant should first completely treat the keloids and ensure there are no signs of recurrence before getting pregnant. Otherwise, there is a high likelihood that the keloids will grow rapidly during pregnancy.
Are keloids hereditary? Will they be passed on to my children in the future?
Actually, keloids are not a genetic disease; they are referred to as having a family history. Genetic diseases are caused by alterations in genetic material, including chromosomal abnormalities and gene mutations that are not visible at the chromosomal level. These diseases are determined entirely or partially by genetic factors and are often congenital, although they can also develop later in life. What is a family history? A family history refers to the occurrence of a particular disease among the family members (a broader range of family members, not limited to direct relatives like grandparents) of a patient. Let's take the two most common diseases as an example: hypertension and diabetes. It is well known that if an elderly person has these conditions, the likelihood of their children developing them is higher, but it is not guaranteed. If the elderly person does not have these conditions, the likelihood of their children developing them is lower, but it is not impossible. If a patient has keloids, the likelihood of their children developing them is higher, but it is not guaranteed. Therefore, keloids are not a genetic disease.
How can hypertrophic scars be prevented?
Hypertrophic scars protrude above the skin surface, significantly affecting aesthetics, and can sometimes be unbearably itchy and painful. So, how can we prevent them? First, protect yourself and try to minimize the chances of getting injured. Second, we need to have a scar prevention mindset. Once an external injury occurs, even if it is minor, such as a pimple, we should handle it seriously and correctly, eliminating inflammation as soon as possible and promoting early wound healing to reduce the rate of hypertrophy. If you accidentally suffer a severe injury, and if your vital signs permit, try to seek professional plastic surgeons for debridement or meticulous cosmetic repair. Follow-up with scar prevention measures to help the injured area recover aesthetically and prevent hypertrophy. For patients with large-area burns, if the burn depth exceeds deep second-degree, it is difficult to avoid hypertrophic scarring. However, by following these points during treatment, good recovery can be achieved. If the trauma is in the hip joint area, pay attention to the positioning of the limbs during the treatment process. After the wound has just healed, promptly go to a professional scar prevention and treatment institution for scar management. Early preventive intervention can nip hypertrophic scars in the bud, making the later recovery smoother and laying a good foundation for complete rehabilitation.
The signs of scar cessation from proliferation
Hypertrophic scars generally enter the maturation and regression phase around 6 months. However, in our many years of clinical observation, we have found that many patients may take up to 1 year or even several years before entering this phase. Therefore, the timing is uncertain and is influenced by many factors such as the patient's constitution, the time of injury, the size, location, and depth of the scar. Once a scar enters the maturation phase, it will no longer grow and can even self-absorb to some extent. Characteristics of a scar entering the maturation phase: - The pain and itching of the scar decrease, the redness subsides, and the color fades. - The scar becomes flatter and softer, and the base loosens. - The most noticeable change is that the color of the scar gradually returns to normal skin tone. If your scar exhibits these characteristics, it indicates that the scar has entered the mature and stable phase and will no longer grow.
Characteristics of the scar proliferation phase
In the early stage of scar hypertrophy, there are a large number of capillaries in the scar tissue, presenting a congested state. Therefore, on the surface, the scar appears red, pink, or purplish-red. During this stage, the main symptoms are pain and itching. Over time, the scar gradually enters the maturation and stabilization phase. In this phase, the congestion of the scar diminishes, the color fades, the scar becomes flatter and softer, and the pain and itching decrease or even disappear. However, the duration of the hypertrophic period is uncertain. For some patients, it may last for several months, while for others, it may take more than a year or even longer. Generally, children and young adults have a longer hypertrophic period, whereas people over 50 years old have a relatively shorter period. Areas with rich blood supply have a longer hypertrophic period, while areas with poor blood supply have a shorter period. Therefore, it is very important to perform early and timely scar prevention.
Bakang Medical
Guidance at Every Step → Your Recovery Journey, Supported.
Bakang Medical
Guidance at Every Step → Your Recovery Journey, Supported.
From your first visit to full recovery, we don't just treat scars—we support you every step of the way.
We know we're not just healing skin, but restoring confidence and hope.
Medical Consultation Email
glhs5966@163.comBeijing Bakang
010-68224472Chengdu Bakang
028-88869988Wuhan Bakang
027-59306430Guangzhou Bakang
020-33976865